Though the United States has only several thousand confirmed cases of COVID-19 as of Tuesday and China hit only 80,000 this year, epidemiologists said the 20% estimate is conservative based on the infection rates that have occurred in prior pandemics. The numbers of infections reported by China and other countries, they said, are surely underestimates since not all infected people are tested or have serious symptoms.
The H1N1 swine flu pandemic of 2009 infected about 60 million Americans over the course of a year, according to federal estimates, with no efforts at social distancing or containment. Scientists are still working to understand exactly how contagious the novel coronavirus is, but current data suggests it appears to be more contagious than the swine flu.
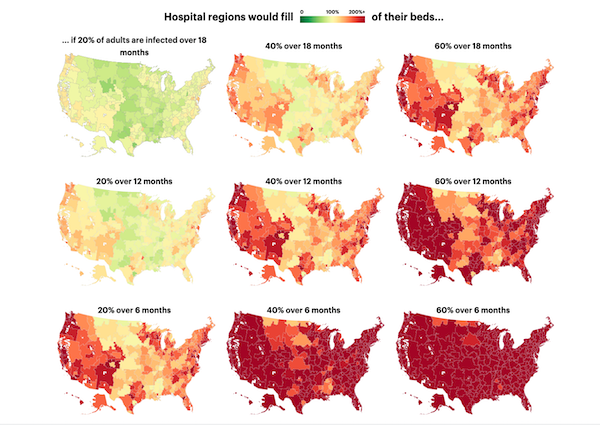
Even in a best-case scenario, with cases of coronavirus spread out over 18 months, American hospital beds would be about 95% full. (This assumes that hospitals don’t free up already occupied beds or add more beds, as some elected officials have called for.) Some regions would have the capacity to handle the surge in hospitalizations without adding new beds or displacing other patients.
But in most other scenarios where the virus spreads faster or infects more people, hospitals would quickly fill their available beds with patients, and they would be forced to either expand capacity, limit elective surgeries and other non-necessary treatments, or make life-and-death decisions about care, similar to what has happened in the worst-hit regions of Italy, where some doctors have received guidance to only treat patients “deemed worthy of intensive care.”
In the Harvard team’s moderate scenario — where 40% of the adult population contracts the disease over the course of a year — 98.9 million Americans would contract the coronavirus, though many will have mild or no symptoms, and will not have their diagnoses confirmed by tests. Slightly more than a fifth of all cases will require hospitalization. (That’s roughly the average number of patients requiring hospitalization in other countries.) To treat all hospitalized patients over that time, the country would have to more than double available hospital beds by freeing up existing beds or adding new ones.
If that moderate estimate holds, about a fifth of hospitalized patients, or nearly 5% of those infected, would become critically ill from COVID-19 and would need intensive care, such as the use of a ventilator.
If all existing ICU beds are freed up for COVID-19 patients, the total capacity would have to be increased 74%. And even then, hospitals may have a limited supply of ventilators and specialized staff who can care for extreme cases.
In the researchers’ worst-case scenario — if 60% of the population falls sick and the virus spreads within six months — the nation would require more than seven times the number of available hospital beds that it currently has.
“Our model gives hospital leaders and policy makers a clear sense of when they will hit capacity and strategic information on how to prepare for rising numbers of patients,” Jha said. “If people wonder ‘Why am I social distancing?’ and ‘Why am I isolating myself?’ this data makes that real. People should look at this data and make sure their community has a plan.”
To be sure, models are based on the best available information and can change over the course of time. And Jha’s model doesn’t take into account the ability of hospitals or states to add additional beds.
Here’s what the situation looks like in Los Angeles:
As of 2018, Los Angeles had 19,500 total hospital beds, of which about 66% were occupied, potentially leaving only 6,590 beds open for additional patients. The bed count includes 2,420 beds in intensive care units, according to data from the American Hospital Association and the American Hospital Directory. Intensive care units are best equipped to handle the most acute coronavirus cases.
The Los Angeles region has a population of about 10 million residents; 12% are over the age of 65. The experience in other countries has shown that elderly patients have significantly higher hospitalization and fatality rates from the coronavirus.
In the moderate scenario, in which 40% of the adult population contracts the disease over 12 months, Los Angeles would be among the regions that would need to expand capacity.
It is estimated that about 8% of the adult population would require hospital care. In a moderate scenario where 40% of the population is infected over a 12-month period, hospitals in Los Angeles would receive an estimated 647,000 coronavirus patients. The influx of patients would require 21,600 beds over 12 months, which is 3.3 times the available beds in that time period. The Harvard researchers’ scenarios assume that each coronavirus patient will require 12 days of hospital care on average, based on data from China.
In the Los Angeles region, intensive care units would be especially overwhelmed and require additional capacity. Without coronavirus patients, there are only 940 available beds on average in intensive care units, which is 4.8 times less than what is needed to care for all severe cases.
For the analysis, Jha and his team selected various rates of infection and modeled hospital capacity for each over three time periods, six months, 12 months and 18 months. The infection rate scenarios are based on estimates from leading epidemiologist Dr. Marc Lipsitch, head of the Harvard T.H. Chan School of Public Health’s Center for Communicable Disease Dynamics, who made the projections of how many people globally would be infected. (Read more about the methodology here.)
By modeling the data over the three time periods, the scenarios illustrate how much the nation could “flatten the curve” with social measures to ensure hospitals have greater capacity to care for coronavirus patients.
“The way to permanently stop new cases from setting off long chains of transmission is to have each case infect considerably less than one case on average,” Lipsitch said. “The numbers will go down. There will still be little outbreaks, but not big ones.”
The data reveals stark regional differences in hospital capacity. Some communities are significantly less equipped to handle surges in medical need.
“A serious epidemic in Grand Forks, North Dakota, will be much different than in Boston,” said Dr. David Blumenthal, president of The Commonwealth Fund, a health care think tank.
Hospitals in more urban communities will likely be more stressed, given the vast populations they serve, but these larger hospital systems may also have more flexibility to stretch their resources by shifting patients around and freeing up beds. For example, hospitals in eastern Long Island, which includes the counties of Nassau, Suffolk and parts of Queens, would need eight times their current available capacity if they don’t rearrange or displace their other patients. But if they freed up all of their existing beds, which are 88% full on average, they would significantly increase their capacity.
New York Gov. Andrew Cuomo has also talked about the need to open up additional hospital beds and has called for the construction of field hospitals to handle the influx of patients.
“You will have people on gurneys in hallways,” Cuomo said at a press conference on Monday, later adding that New York would need up to 110,000 total hospital beds, around twice the number it currently has. “That is what is going to happen now if we do nothing.”
Not all communities will have the depth of resources to draw on.
On Maryland’s Eastern Shore, Salisbury is one of the communities at the highest risk of being under capacity, even if it frees up all of its beds for coronavirus cases, according to our analysis of the Harvard researchers’ data. The researchers estimate that in a moderate infection scenario, the community will have about 149,000 coronavirus cases.
If the community is able to spread infections over 12 months, it would have to add about 880 beds to treat all adult coronavirus patients, either by building new beds or discharging existing patients, which is more than four times its current capacity of 187 available beds. Even if it released all of its existing patients and replaced them with coronavirus cases, it would still need to nearly double the number of beds.
Fran Phillips, deputy secretary for Public Health Services for Maryland’s Department of Health, said at a Monday press conference that her office is working to nearly double the capacity of the state’s hospitals to meet the expected surge in patients.
The hospital system in Santa Cruz only has 22 intensive care unit beds, of which on average only 30% are available on any given day. To care for all critically ill coronavirus patients over a 12-month period without kicking out other critically ill patients, the hospital system would have to increase its ICU capacity by 2,133%, or 128 more beds, according to the analysis.
Dignity Health, which manages four nonprofit hospitals in the Bay Area, including Dominican Hospital in Santa Cruz, said in an email through spokesperson Felicity Simmons that the company is continuously updating its capacity procedures to meet patient demands. The company has considered adding medical tents outside of the hospital for additional triage and treatment, and patients could “also be transferred to our sister facilities or to other nearby health systems.”
Some hospital systems, particularly those in more rural or unpopulated communities, may have greater capacity to deal with the influx of patients, according to the model. In Minot, North Dakota, 9,300 adult residents would likely be hospitalized if 40% of the population is infected over a 12-month period. Unlike most other regions, its current supply of hospital beds should be enough to care for all patients. But hospital capacity is not all that matters, Jha said. For example, remote facilities may have less experienced staff and less specialized equipment to care for complex cases.
Karim Tripodina, a spokeswoman with Trinity Health, which runs the largest hospital in Minot, said in an email that the facility is prepared. “We all work with our health care partners across the region and depend on the system as a whole to respond to the needs of any of its parts.”
Dr. Lewis Nelson, a professor and chair of the Department of Emergency Medicine at Rutgers University New Jersey Medical School, believes that part of the reason we’re likely to see such stark hospital bed shortages is because so many hospitals have closed in recent years. The bed shortages, he said, could force critical care doctors to bend the accepted standards of care.
“We will have to make these hard decisions,” he said, such as whether some patients receive high-level treatment and others don’t. “They will be personal decisions and they run counter to how health care is practiced in this country.”
When doctors at the University of California, San Francisco, began to see their first cases of COVID-19 in February, administrators quickly recognized that they might not have the resources to treat all the patients they were likely to see. According to the Harvard scenario where 40% of adults in the country contract the disease, about half a million people in the San Francisco region may get infected, with more than 100,000 residents requiring hospitalization. If the infections occur over a 12-month period, the city would need three times the number of available hospital beds and ICU beds it has.
“We realized that we did not have the capacity to put all the suspected patients into private rooms,” said Dr. Maria Raven, chief of emergency medicine at UCSF and vice chair of the emergency medicine department at Zuckerberg San Francisco General Hospital. In the past, “on occasion we had to have folks out in hallways with masks on.”
Within a week of the first confirmed infections in the city, the hospital erected two temporary medical tents to screen and treat potentially infected patients. The goal is to keep the number of patients seen at the hospital to a manageable level.
“Seeing what’s going on in other countries, we are all preparing for a potential tidal wave of patients,” said Dr. Jeanne Noble, an emergency care physician in charge of coronavirus response at UCSF. “We feel like we’re teetering on the edge of a cliff.”
For hospitals with fewer resources, there are measures that can be taken to counter bed shortages. Hospitals can limit elective surgeries and discharge healthier patients earlier. Hospitals can also screen patients before they enter the hospital to decrease the risk of spreading the disease. Critically, staffers also need to stay healthy, so they can continue to treat patients instead of taking up the needed beds themselves.
The experts and health workers that ProPublica spoke with fear that the U.S. is only two weeks behind Italy’s infection rate and will be faced with the same tough decisions. A paper published in the Lancet last week highlighted Italy’s Lombardy region, where a flood of patients is overwhelming the intensive care system.
“I can’t imagine being in that position, and none of us want to be in that position,” said UCSF’s Raven. “The reality is that you can’t create unlimited hospital beds and ventilators. We have what we have, so we really have to hope that it’s enough, and that we’re prepared enough.”

West Hollywood is doing nothing to enforce stay at home guidelines or wearing masks. It’s like Alice in wonderland in Weho. Not to mention the lost month before Weho started to take is seriously
To the contributors of this article, thank you for the information. It is a difficult situation but details and data are real. Be safe.
One particular love/hate about Los Angeles, is in normal times MOST people drive everywhere, have larger homes with more space, and compared to NY, the lyfestyle that is loved & criticized may be a big help in a lower rate than most Big Cities where almost ALL rely on some form of public transportation. (I don’t drive) ALSO Cedars-Sinai is on the short list of Worlds Greatest Hospitals. Over the last 15 or so years, Cedars (like all major hospitals) did a big building expansion. THEY calculated the baby boomer generation was the first to have ENORMOUSLY LO HER LIFE… Read more »